Trek for Strategic Market Entry
Strategic M&A: Expand into New Markets with Confidence
Evaluate expansion and M&A opportunities with a clear view of local reimbursement dynamics and payer mix. Better understand service line growth opportunities while aligning new offerings to market benchmarks before scaling operations.
Expansion Intelligence has Leveled Up
Leverage expansion-ready data that turns payer transparency into clear go-to-market strategies.
Accurate Market Entry Intelligence
Leverage market data to profitable expansions.
Service Line Growth
Target high-margin specialty opportunities for faster growth.
M&A Valuation & Post-Deal
Standardize rates to strengthen system-wide leverage.
Powering the Three Pillars of Market Expansion
Successful market expansion requires more than ambition. Provider organizations need a data-driven strategy, targeted growth initiatives, and disciplined risk management to enter new markets with confidence and sustain long-term success.
Market Readiness
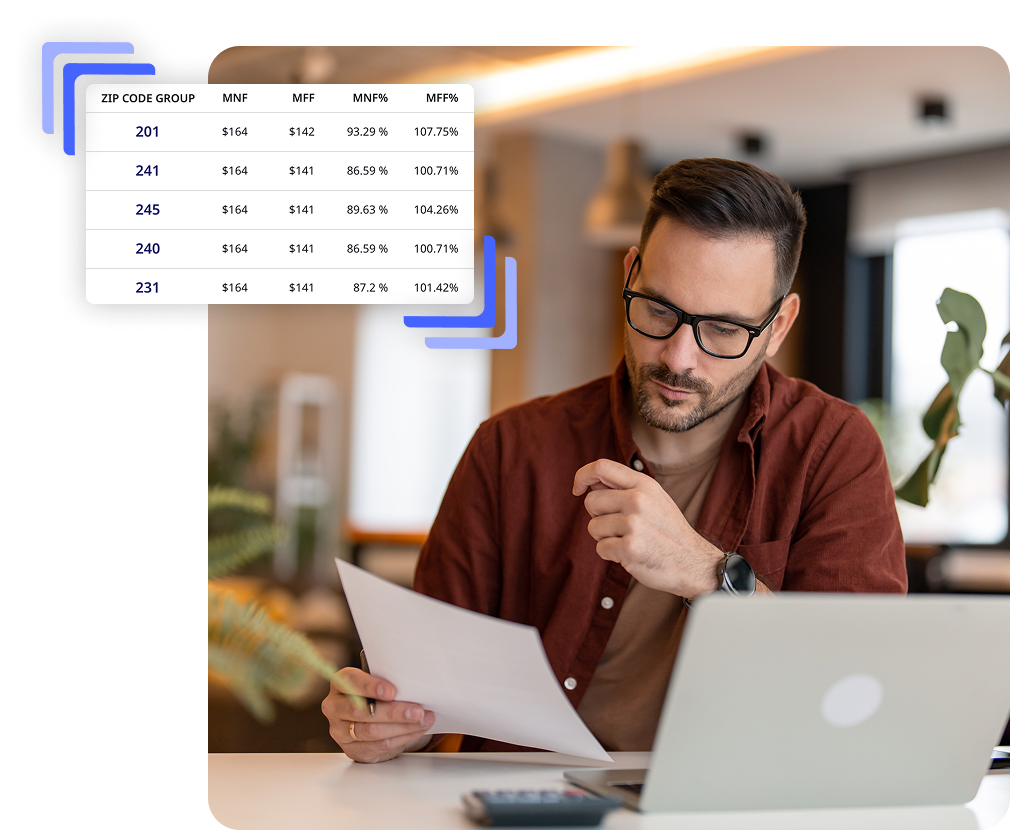
- Analyze competitors, reimbursement levels, and payer networks
- Benchmark potential acquisitions against local and regional averages
- Ensure new entities align with market benchmarks from day one

Service Line Growth
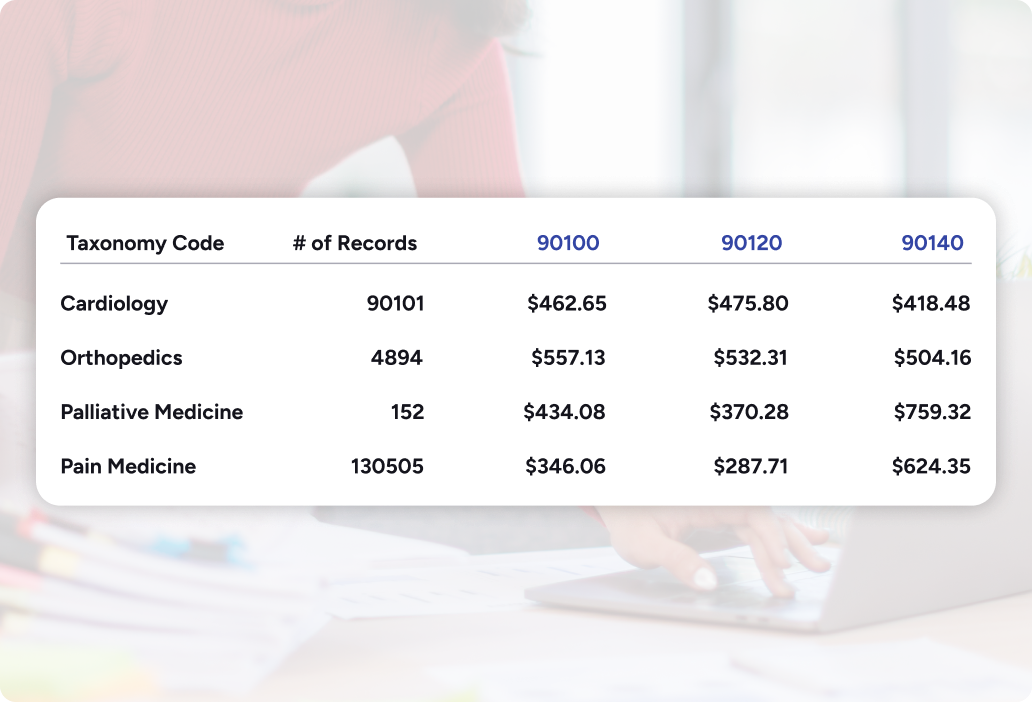
- Benchmark reimbursement across target service lines
- Pinpoint high-margin opportunities with strong revenue potential
- Uncover underserved service lines with limited competition

Sustained Market Performance
- Align proposed rates with competitive benchmarks
- Focus expansion on proven, high-return opportunities
- Monitor post-entry performance and refine strategies
Transparency Solutions for Every Stage of Expansion
Whether you are entering into a new market with an acquisition or a new facility, Trek’s data allows you to feel confident you are making the right decision for financial sustainability.


Contract Intelligence
Embed negotiation-ready intelligence into contract management workflows to streamline expansion planning, accelerate post-acquisition integration, and deliver measurable revenue impact.



Price Intelligence
Transform verified payer and market data into powerful intelligence that benchmarks your position, uncovers hidden revenue, and drives sustainable margin growth.

Market Expansion Resources

Competitive Market Analysis (CMA): Outperform Every Negotiation
Get a clear, high-level view of how your organization performs against the market, starting with a visual performance dashboard. Then drill down into competitive benchmarks to uncover revenue opportunities and guide targeted contract strategies.
- Compare reimbursement across markets, payers, and service lines to identify areas of underperformance
- Target high-impact negotiation opportunities backed by competitor-specific proof points
- Support market expansion decisions with validated performance data
- Build a negotiation narrative anchored in competitive advantage

Rate Change: Track and Act on Market Movement
Monitor quarter-over-quarter reimbursement changes for your organization and competitors to identify patterns, pinpoint anomalies, and forecast the financial impact of rate shifts.
- Detect downward trends early to protect revenue before renewals
- Validate payer claims and rate changes with historical data
- Highlight positive trends to reinforce payer relationship and maintain gains
- Guide long-term contract strategy with multi-year rate performance analysis


Frequently Asked Questions
How does Trek Health identify service line growth opportunities?

Trek Health identifies high-margin specialties and uncovers underserved service lines by leveraging verified payer and market data.
How does the platform ensure long-term success after entering a new market?

By monitoring reimbursement trends, payer mix, and competitive benchmarks, Trek Health helps organizations refine strategies and sustain financial performance.
Why should provider organizations use payer transparency data for market expansion?

Payer transparency data provides accurate, real-time visibility into local reimbursement dynamics, helping leaders reduce risk and expand with confidence.



.png)
.png)
