
Inside Trek Health’s Competitive Market Analysis (CMA) Tool
Inside Trek Health’s Competitive Market Analysis (CMA) Tool
In the era of price transparency, health systems don’t just need more data—they need sharper tools. That’s why Trek Health’s newest product release, Competitive Market Analysis (CMA), is designed to help provider organizations navigate complex rate data with confidence, clarity, and speed.
Why CMA?
Payer transparency regulations have opened the floodgates to an overwhelming amount of pricing data. But raw files alone won’t improve your bottom line. Trek Health’s CMA tool transforms those datasets into negotiation-ready insights—so you can stop guessing and start leveraging.
Built to augment, not replace, your existing teams, CMA delivers intuitive visualizations, AI-powered insights, and customizable views that eliminate manual work and accelerate strategy.
What’s Inside CMA
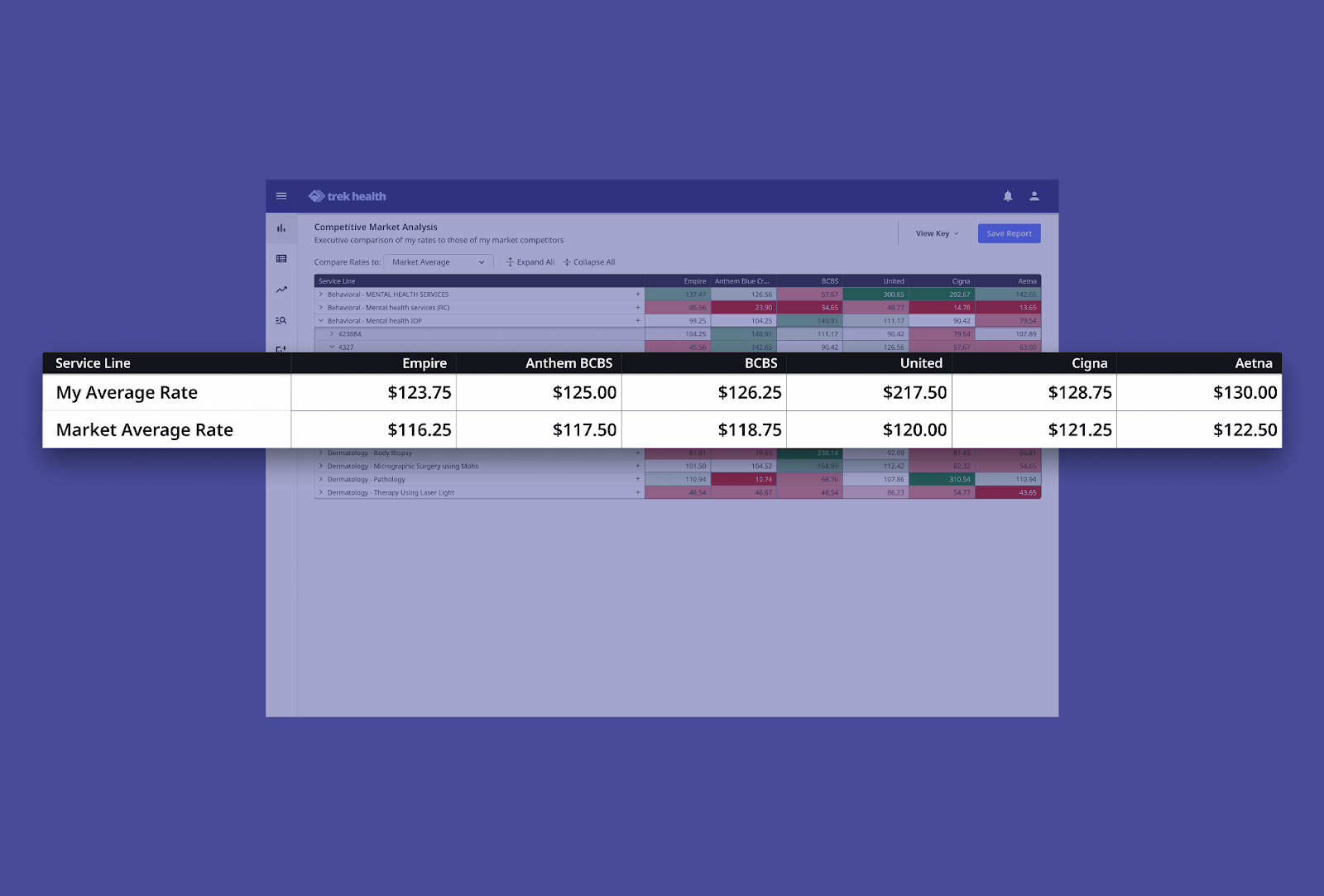
1. Real-Time Market Benchmarking
Get up-to-date comparisons of your contracted rates against the competition—down to the service line or payer level.
2. Custom Views by Service Line & Payer
No more generic dashboards. CMA filters let you drill down into exactly what matters, whether by CPT code, location, or payer.

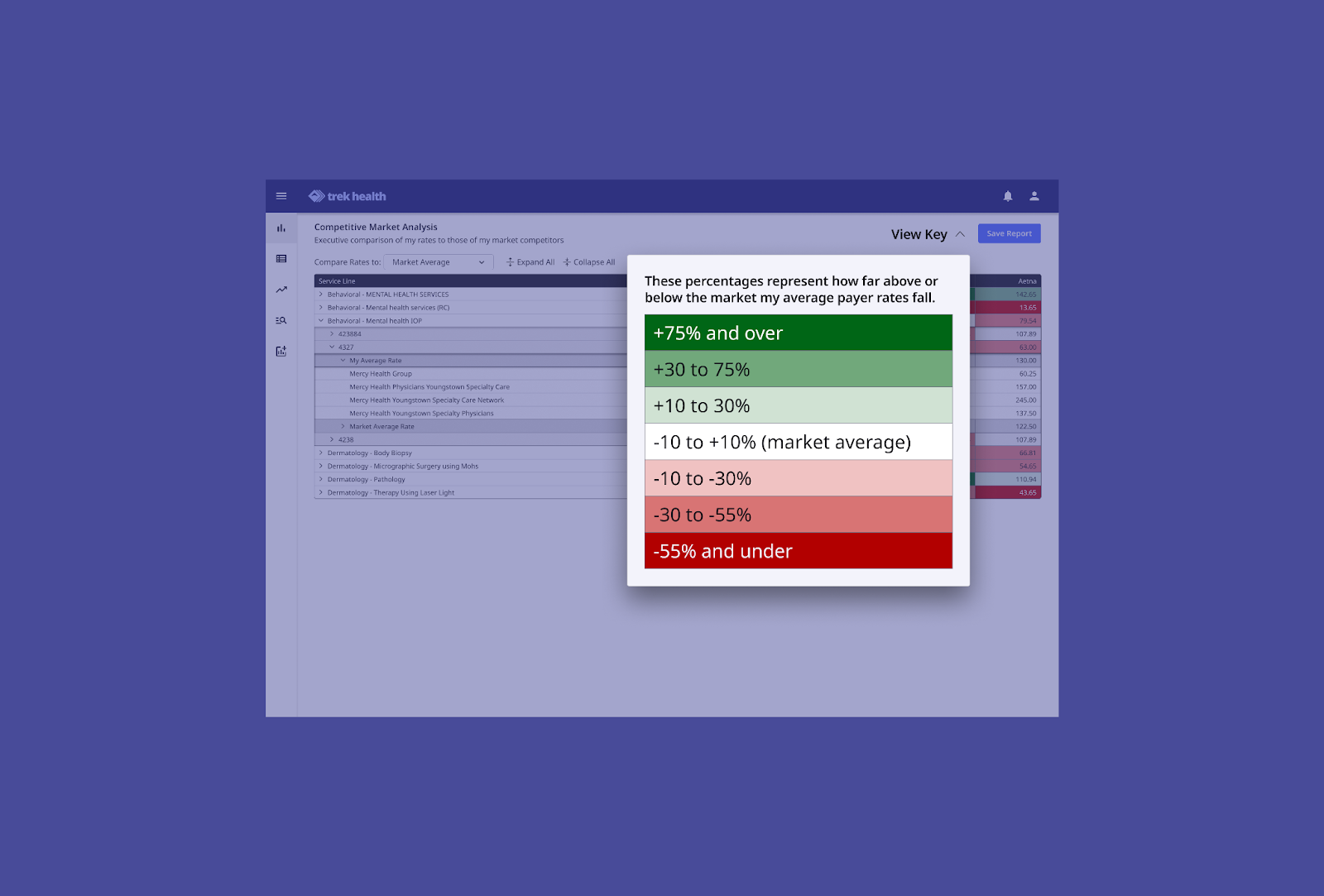
3. Visual Heatmaps That Surface Opportunity
With a glance, know where you're outperforming (green), underperforming (red), or sitting at the market average (white). These heatmaps turn rate data into instant leverage.
What CMA Delivers for Health Systems
Revenue Intelligence
CMA gives executives a high-level view of performance, while also providing the detail needed to act.
- Assess your market position
- Identify strengths and gaps
- Spot payer or service-line trends
- Make fast, informed decisions
Key Features
- Data Transparency: Side-by-side rate comparisons
- Heat Map Visualization: Quickly spot wins and weaknesses
- Customizable Filters: Slice data by location, service line, payer
- Real-Time Data: Always current, always ready
- Actionable Intelligence: Convert raw data into strategy
Provider Benefits
With CMA, provider organizations gain:
- Informed Negotiations: Walk into payer conversations with full market context
- Revenue Optimization: Quickly identify and fix underperforming contracts
- Competitive Advantage: Stay ahead with real-time insights
- Efficient Decision-Making: Visuals simplify complex data
- Strategic Planning: Use CMA to guide both immediate and long-term strategy
What Users Are Saying
As payer transparency continues to reshape healthcare in 2025, CMA is the go-to tool for rate benchmarking. It reduces time spent gathering data, so your teams can focus on analysis, modeling, and strategy.
By simplifying complex comparisons and surfacing negotiation leverage in real time, CMA helps contracting teams work faster—and smarter.
Here’s what Paul Greenspan from Sandstone Care had to say:

Want Smarter Negotiations?
Trek’s CMA is already helping health systems nationwide turn payer-posted data into a strategic advantage. Whether you’re in managed care, finance, or legal, CMA ensures everyone’s aligned—on one platform, with one source of truth.
🔍 Schedule a demo to see CMA in action.
📲 Follow Trek Health on LinkedIn to stay ahead in the transparency era.
.png)
White Paper
From Transparency to Prediction: Quantifying the Drivers of Physician Reimbursement Variation
This analysis uses Transparency in Coverage data to model how payers behave, not just what they pay. By linking reimbursement rates to physician characteristics, we uncover the patterns behind payment variation and transform transparency data into predictive intelligence. The result: a predictive view of rate dynamics that helps stakeholders anticipate trends and negotiate with data-driven confidence.

White Paper
Q3 2025 State of Commercial Reimbursement: Trek Health’s Quarterly Market Intelligence
Trek Health’s Quarterly Reimbursement Brief highlights emerging variability in commercial payment rates across U.S. payers, specialties, and geographic markets. With some segments experiencing double-digit growth and others notable declines, contracting performance is increasingly shaped by real-time payer behavior rather than historical norms. Through validated reimbursement trend analytics, contract intelligence, and policy monitoring, Trek equips provider organizations to anticipate market shifts, protect revenue, and negotiate with measurable leverage.

White Paper
Q4 2025 State of Commercial Reimbursement: Trek Health’s Quarterly Market Intelligence
Trek Health’s Q4 2025 Quarterly Market Intelligence report analyzes quarter-over-quarter commercial reimbursement movement across national payers, physician specialties, and U.S. states. While overall reimbursement improved following earlier declines, rate changes remained uneven—highlighting payer selectivity, persistent specialty outliers, and shifting geographic leverage. This report moves beyond static benchmarks by tracking real-time reimbursement changes, giving provider organizations actionable insight to identify negotiation risk early, protect rate parity, and respond proactively to evolving payer behavior.

White Paper
Reimbursement and Reality: The Economics of Breast Cancer Treatment
While breast cancer awareness efforts often focus on screening and treatment, one critical factor remains overlooked: how care is reimbursed. Payment structures shape far more than provider margins; they influence access, equity, and patient outcomes.
In this analysis of payer rates, Trek Health uses its Transparency Platform to analyze how reimbursement for breast cancer care varies across geography, commercial payer behavior, and public policy. The findings reveal a system that rewards disease burden rather than prevention which creates inequities that ripple through the entire care process.
Inside you’ll learn:
- How reimbursement rates differ dramatically by state and payer
- Why higher disease burden correlates with higher payment, but prevention does not
- What these trends mean for provider strategy, patient access, and equity
Download the full analysis to see how transparency data can help reshape breast cancer care—turning financial insight into fairer outcomes.

White Paper
The Economics of Payer Contract Management Automation: Quantifying Cost Savings & Revenue Lift
Trek Health's Contract Intelligence (CI) automates contract interpretation and policy maintenance, transforming unstructured payer data into actionable rules. Using industry benchmarks and multi-scenario modeling across clinic, multispecialty, and hospital environments, CI generates annual savings ranging from $80K to over $9.3M, driven by avoided denials, reduced administrative labor, and streamlined policy-update workflows. Our results show that CI functions as core financial infrastructure rather than a point solution, delivering structural value across the reimbursement lifecycle.

White Paper
The Payer Paradox: When Higher Rates Don’t Mean Higher Reimbursement
This analysis uncovers a critical paradox in commercial healthcare financing: the payers offering the highest contracted rates often deliver the lowest realized reimbursement once denials and administrative friction are accounted for. By introducing the Payer Generosity Index (PGI) and adjusted PGI (aPGI), Trek Health reveals how payer performance varies not only across insurers, but across specialties and service lines. These findings equip healthcare organizations with a clearer, data-driven framework for contracting, revenue optimization, and strategic planning in an increasingly complex reimbursement landscape.

White Paper
The Private Practice Playbook: Rate Negotiation Index Rankings for Specialty-Specific M&A Strategy
Physician economics are shifting as private equity and independent platforms redefine the workforce landscape. Trek Health’s Rate Negotiation Index Report quantifies the return on physician labor across states and specialties in a new lens: combining commercial reimbursement, physician salary, malpractice risk, and provider density into a single metric. This data driven foundation for smarter M&A strategy identifies the most economically sustainable opportunities across the U.S. for physician recruitment and network expansion.

Published on
July 8, 2025
Written by
Inside Trek Health’s Competitive Market Analysis (CMA) Tool
In the era of price transparency, health systems don’t just need more data—they need sharper tools. That’s why Trek Health’s newest product release, Competitive Market Analysis (CMA), is designed to help provider organizations navigate complex rate data with confidence, clarity, and speed.
Why CMA?
Payer transparency regulations have opened the floodgates to an overwhelming amount of pricing data. But raw files alone won’t improve your bottom line. Trek Health’s CMA tool transforms those datasets into negotiation-ready insights—so you can stop guessing and start leveraging.
Built to augment, not replace, your existing teams, CMA delivers intuitive visualizations, AI-powered insights, and customizable views that eliminate manual work and accelerate strategy.
What’s Inside CMA
1. Real-Time Market Benchmarking
Get up-to-date comparisons of your contracted rates against the competition—down to the service line or payer level.
2. Custom Views by Service Line & Payer
No more generic dashboards. CMA filters let you drill down into exactly what matters, whether by CPT code, location, or payer.

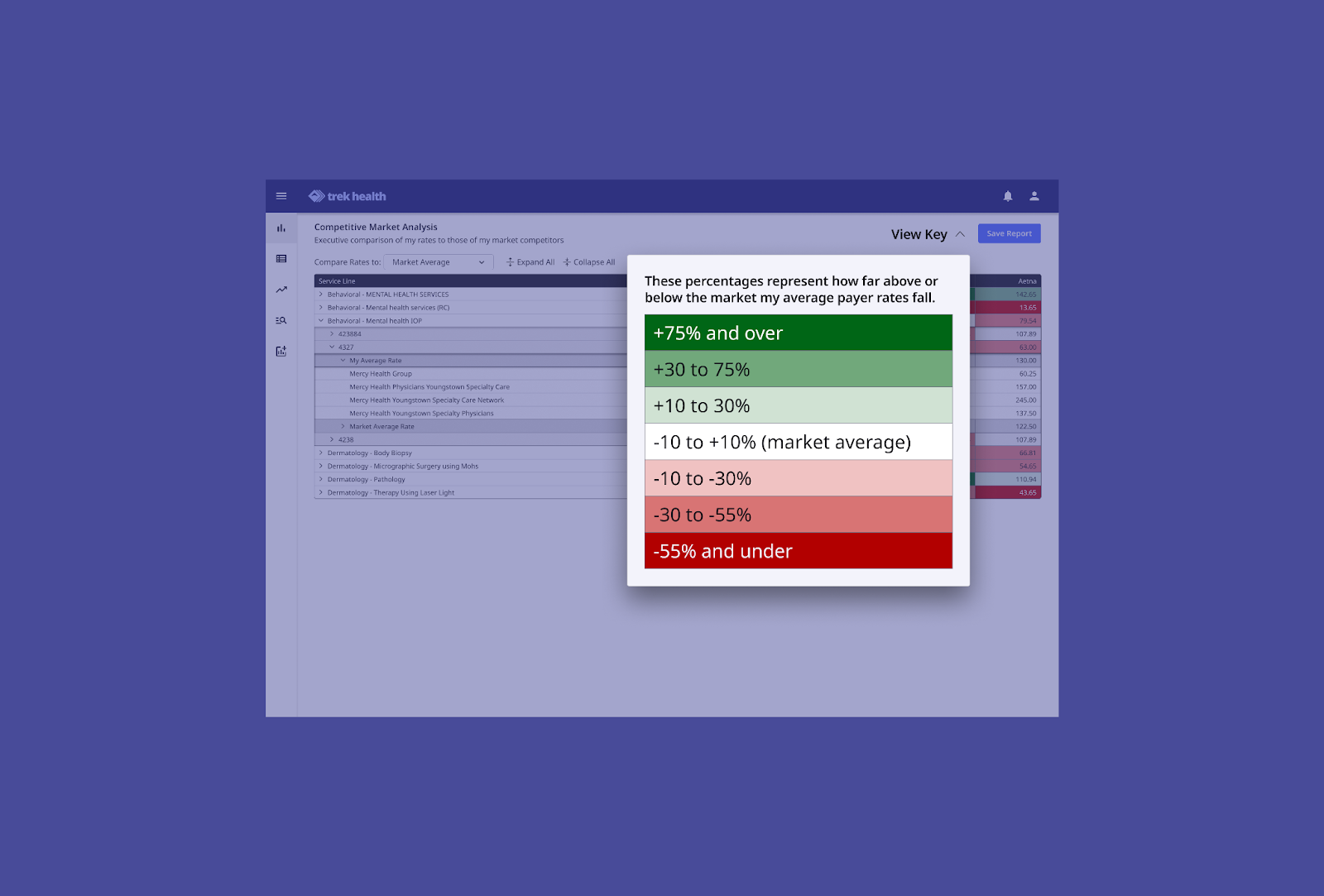
3. Visual Heatmaps That Surface Opportunity
With a glance, know where you're outperforming (green), underperforming (red), or sitting at the market average (white). These heatmaps turn rate data into instant leverage.
What CMA Delivers for Health Systems
Revenue Intelligence
CMA gives executives a high-level view of performance, while also providing the detail needed to act.
- Assess your market position
- Identify strengths and gaps
- Spot payer or service-line trends
- Make fast, informed decisions
Key Features
- Data Transparency: Side-by-side rate comparisons
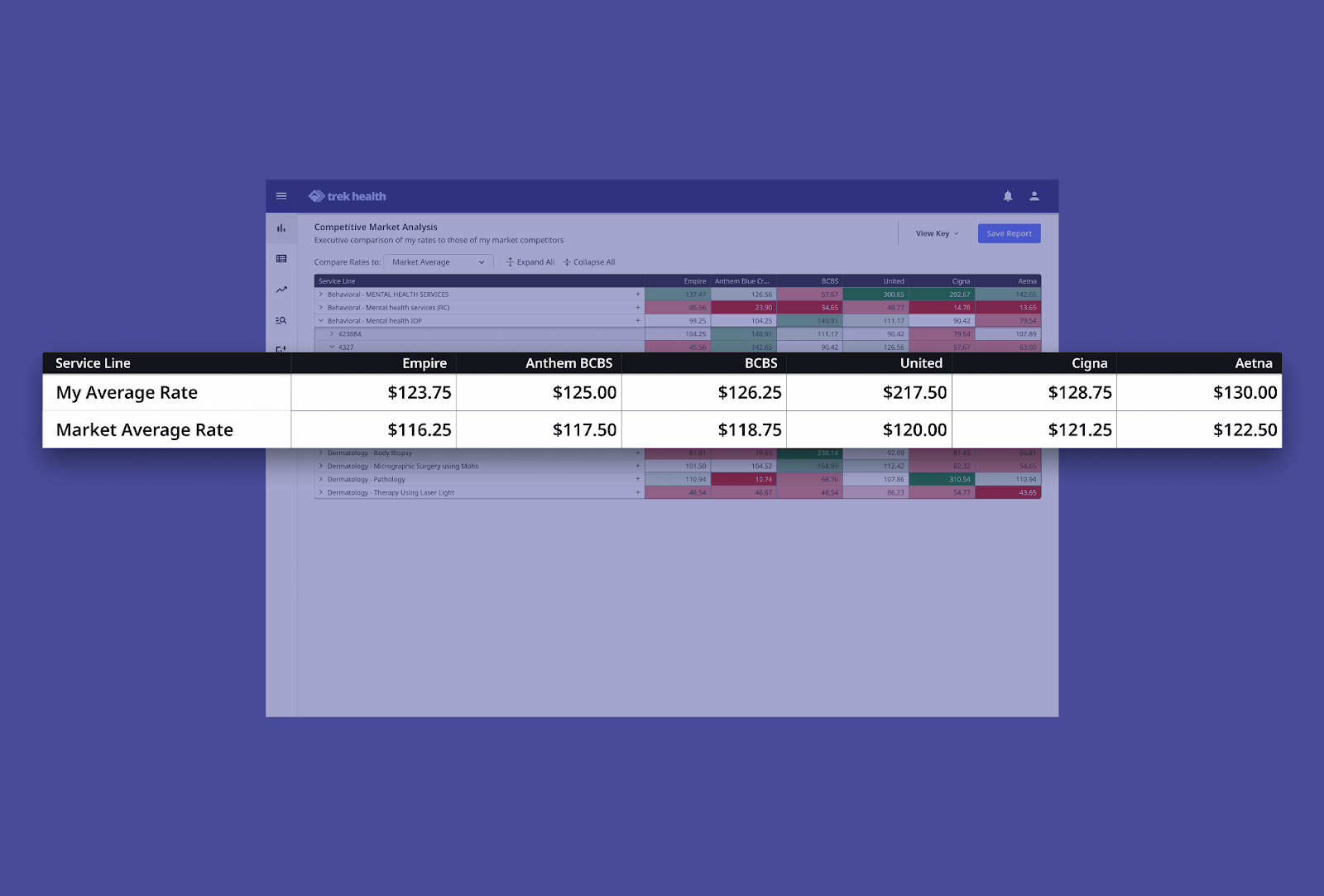
- Heat Map Visualization: Quickly spot wins and weaknesses
- Customizable Filters: Slice data by location, service line, payer
- Real-Time Data: Always current, always ready
- Actionable Intelligence: Convert raw data into strategy
Provider Benefits
With CMA, provider organizations gain:
- Informed Negotiations: Walk into payer conversations with full market context
- Revenue Optimization: Quickly identify and fix underperforming contracts
- Competitive Advantage: Stay ahead with real-time insights
- Efficient Decision-Making: Visuals simplify complex data
- Strategic Planning: Use CMA to guide both immediate and long-term strategy
What Users Are Saying
As payer transparency continues to reshape healthcare in 2025, CMA is the go-to tool for rate benchmarking. It reduces time spent gathering data, so your teams can focus on analysis, modeling, and strategy.
By simplifying complex comparisons and surfacing negotiation leverage in real time, CMA helps contracting teams work faster—and smarter.
Here’s what Paul Greenspan from Sandstone Care had to say:

Want Smarter Negotiations?
Trek’s CMA is already helping health systems nationwide turn payer-posted data into a strategic advantage. Whether you’re in managed care, finance, or legal, CMA ensures everyone’s aligned—on one platform, with one source of truth.
🔍 Schedule a demo to see CMA in action.
📲 Follow Trek Health on LinkedIn to stay ahead in the transparency era.

