

Price Intelligence
Strengthen Payer Strategies with Actionable Market Insights
Gain a clear, validated view of how commercial reimbursement rates vary across payers, markets, and service lines.
Actionable Insights for Smarter Negotiations
Evolve from reactive reporting to proactive, data-driven decisions that enhance payer performance and safeguard margins.
Leverage an actionable and up-to-date commercial payer data set refreshed each quarter
Analyze competitive positioning with market-level comparisons and visual benchmarks.
Track reimbursement shifts over time to detect trends, anomalies, and opportunities
Identify underpayments and rate gaps to recover lost revenue and identify growth opportunities.
Reimbursement Insights
Build a precise, data-driven understanding of how your organization is reimbursed across every payer and service line. Uncover rate disparities, validate negotiation positions, and quantify where improved terms can deliver the greatest margin impact.





Rate Research: Provider-Level Rate Visibility
Drill into your organization’s specific reimbursement across multiple billing codes, organized by taxonomy and region.
- Pinpoint provider-level rate discrepancies to target negotiation opportunities
- Avoid outdated rates by validating against payer-published data
- Monitor changes in reimbursement over time to maintain competitive positioning
- Support service line and market strategies with detailed provider-specific insights

Group Rate Research: System-wide Rate Intelligence
Understand how your organization is reimbursed across payers, billing codes, and locations to uncover variations and drive stronger, enterprise-wide negotiation strategies.
- Drive uniform, higher-performing contracts that lift revenue across the enterprise
- Eliminate missed renegotiation opportunities with a single, system-wide view of payer performance
- Maximize negotiation leverage with consolidated, organization-level rate intelligence
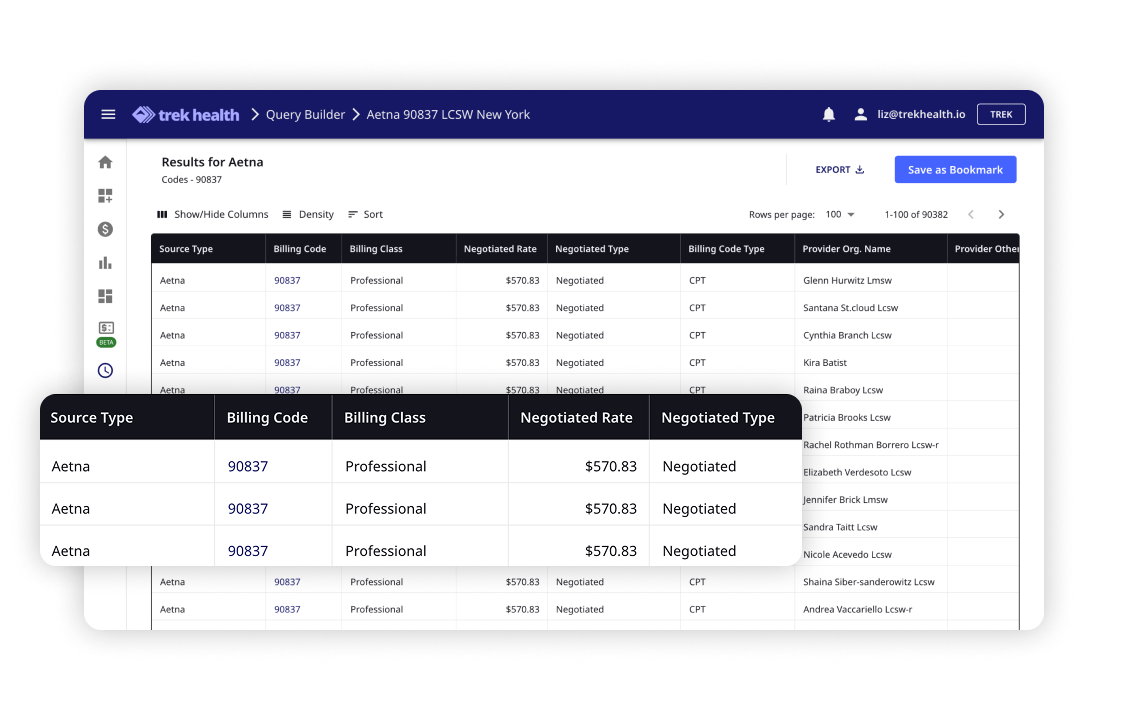
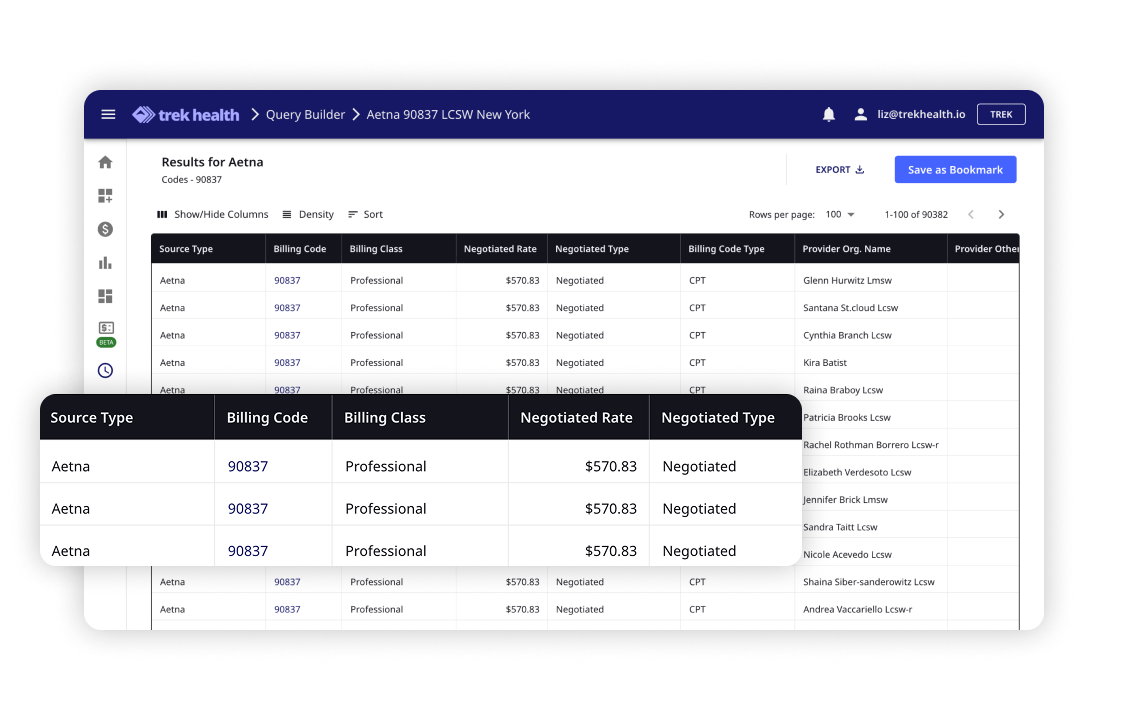
Query Builder: Custom Analytics Without Limits
Build tailored, filter-based searches across raw payer rate data to generate detailed exports and empower in-house analysis and modeling.
- Accelerate high-value negotiations with payer-specific rate intelligence
- Quantify the financial upside of contract adjustments before discussions begin
- Discover hidden rate patterns that drive immediate revenue gains
- Reduce dependencies on outside consultants by empowering in-house analytics

Benchmark Report: Compare, Rank, and Win Better Rates
Analyze average reimbursement rates for specific procedures across defined markets to identify outliers, compare against market percentiles, and target improvement areas.
- Increase reimbursement by targeting payers with below-market rates
- Use percentile rankings to justify higher rates and secure stronger contract terms
- Focus negotiation efforts on ZIP codes or specialties with the highest revenue upside

Competitive Analysis: Understand and Outperform the Market
Compare a provider organization’s reimbursement rates directly against competitors to identify where others earn more for identical services.
- Win higher reimbursement by showing payers where competitors are paid more
- Close rate gaps in profitable service lines to unlock measurable revenue
- Redirect payer dollars to your system by demonstrating market inequities in your favor
- Validate strategy with competitor-specific proof points
Market Insights
Gain clarity into how your organization performs within the broader reimbursement landscape. Identify market trends, track payer behavior over time, and pinpoint opportunities to strengthen competitiveness and protect long-term revenue stability

Competitive Market Analysis (CMA): Outperform Every Negotiation
Get a clear, high-level view of how your organization performs against the market, starting with a visual performance dashboard. Then drill down into competitive benchmarks to uncover revenue opportunities and guide targeted contract strategies.
- Compare reimbursement across markets, payers, and service lines to identify areas of underperformance
- Target high-impact negotiation opportunities backed by competitor-specific proof points
- Support market expansion decisions with validated performance data
- Build a negotiation narrative anchored in competitive advantage

Rate Change: Track and Act on Market Movement
Monitor quarter-over-quarter reimbursement changes for your organization and competitors to identify patterns, pinpoint anomalies, and forecast the financial impact of rate shifts.
- Detect downward trends early to protect revenue before renewals
- Validate payer claims and rate changes with historical data
- Highlight positive trends to reinforce payer relationship and maintain gains
- Guide long-term contract strategy with multi-year rate performance analysis



Competitive Market Analysis (CMA): Outperform Every Negotiation
Get a clear, high-level view of how your organization performs against the market, starting with a visual performance dashboard. Then drill down into competitive benchmarks to uncover revenue opportunities and guide targeted contract strategies.
- Compare reimbursement across markets, payers, and service lines to identify areas of underperformance
- Target high-impact negotiation opportunities backed by competitor-specific proof points
- Support market expansion decisions with validated performance data
- Build a negotiation narrative anchored in competitive advantage

Rate Change: Track and Act on Market Movement
Monitor quarter-over-quarter reimbursement changes for your organization and competitors to identify patterns, pinpoint anomalies, and forecast the financial impact of rate shifts.
- Detect downward trends early to protect revenue before renewals
- Validate payer claims and rate changes with historical data
- Highlight positive trends to reinforce payer relationship and maintain gains
- Guide long-term contract strategy with multi-year rate performance analysis


Frequently Asked Questions
Can provider organizations use Price Intelligence to benchmark reimbursement rates across regions and specialties?

Yes. The platform enables filtering by provider, payer, geography, specialty, and billing code. This enables leaders to compare reimbursements across facilities and service lines, identify rate variations, and target the highest-value opportunities for contract improvement.
How accurate and reliable is the rate intelligence provided in the platform?

All data is pulled directly from payer-published MRFs and updated quarterly to ensure accuracy and reliability. Trek validates rates against source files to eliminate outdated information and provide healthcare executives with verified, market-level intelligence.
What types of insights can healthcare finance teams gain from Price Intelligence and how can that help with negotiations?

Healthcare finance and strategy teams can identify underpayment risks, track reimbursement trends over time, quantify the financial benefits of contract adjustments, and benchmark performance against competitors, which can help validate negotiation positions. These insights directly support payer negotiations, market expansion, physician recruitment, and long-term financial planning and decision-making.
What is Competitive Market Analysis (CMA), and how does it benefit provider negotiations?

CMA provides a high-level performance dashboard that compares your reimbursement against market averages and competitor benchmarks. It highlights underpayment risks, uncovers negotiation opportunities, and offers payer-facing proof points that strengthen contract strategy and financial outcomes.
Can Price Intelligence help identify underpayments and revenue leakage?

Yes. The platform surfaces rate gaps and underpayments by comparing reimbursement performance against verified payer-published data. This enables finance leaders to quantify lost revenue, validate payer claims, and recover earnings that may otherwise go unaccounted for.
Why should healthcare finance teams use Price Intelligence instead of relying solely on claims data?

Claims data shows past reimbursement but lacks complete visibility into market-wide payer rates. Prince Intelligence leverages payer-published transparency data to provide a broader and more accurate view of competitive positioning, enabling leaders to proactively negotiate, optimize contracts, and guide strategic growth decisions.





