
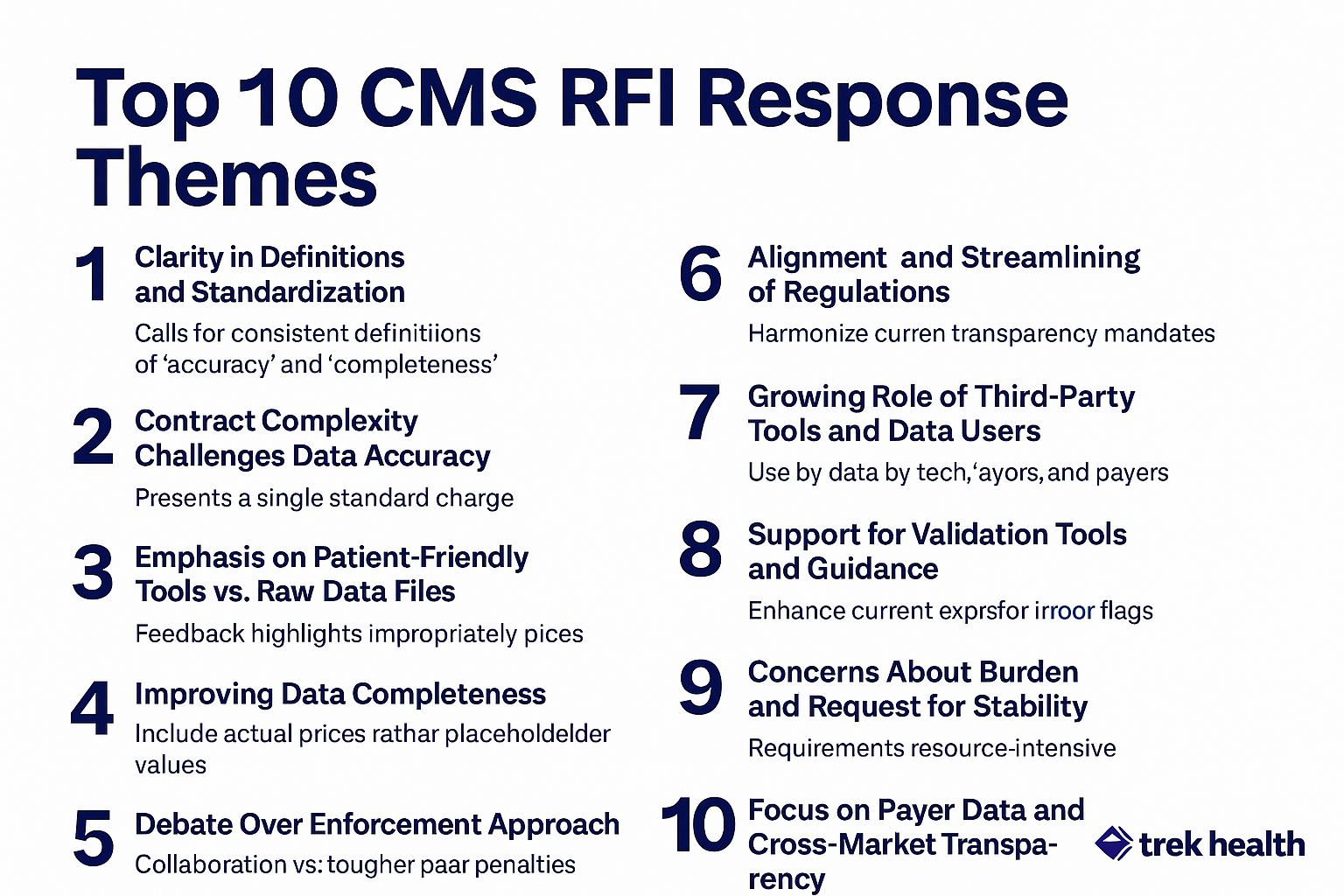
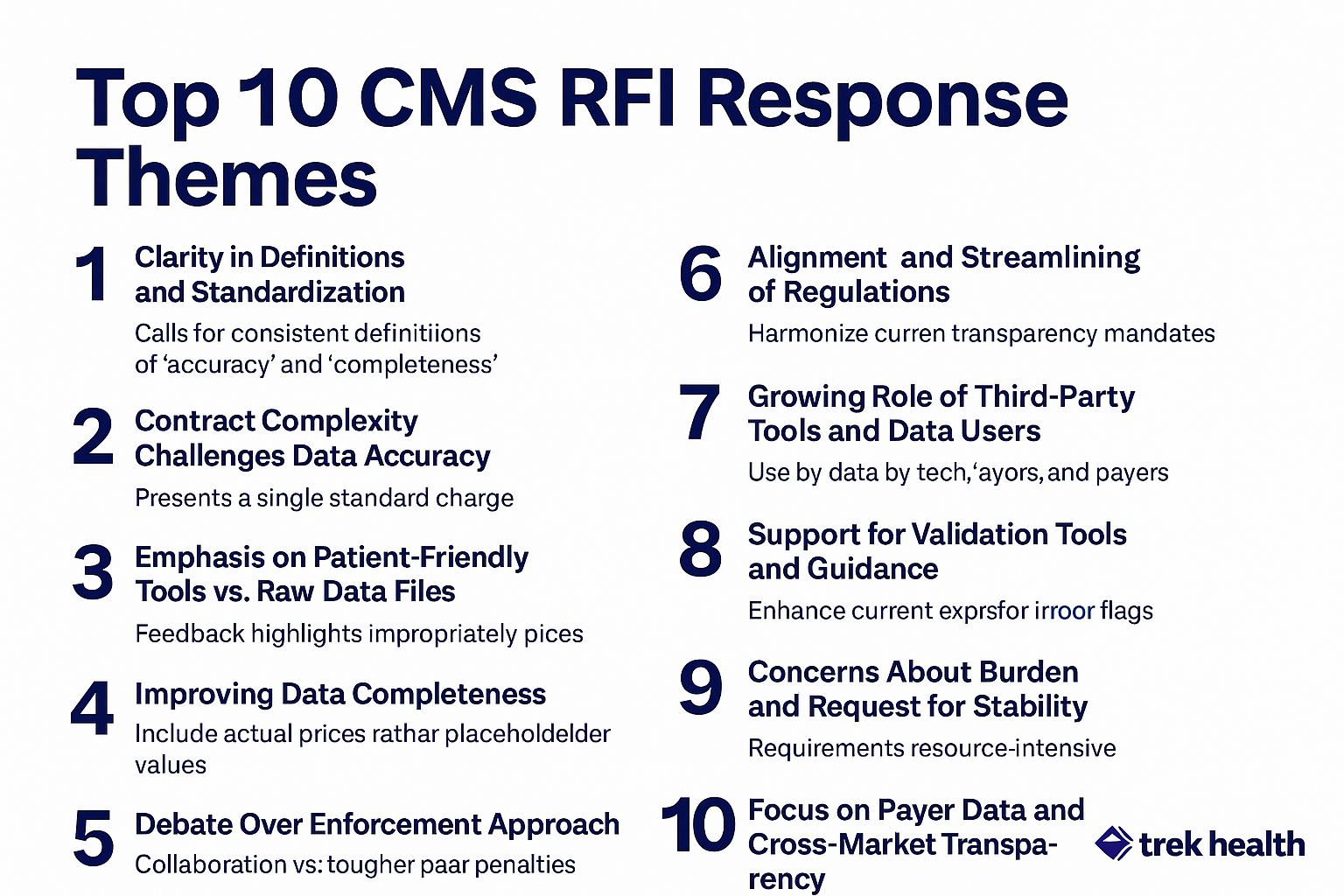
The Top 10 CMS RFI Response Themes and What They Mean for Price Transparency
The Top 10 CMS RFI Response Themes and What They Mean for Price Transparency
As CMS moves to refine and enforce hospital price transparency rules, the agency's Request for Information (RFI) drew an important response from stakeholders across the healthcare ecosystem. Hospitals, tech vendors, employers, patient advocates, and consultants all weighed in, and while not everyone agrees on the how, the what is clear: there's a new wave of transparency that prioritizes consistency, usability, and accountability.
Below, we break down the top 10 themes from the CMS RFI responses and what they signal for health systems trying to stay compliant, strategic, and ahead of enforcement.
1. Clarity in Definitions and Standardization
Across the board, stakeholders urged CMS to define key terms like "accuracy" and "completeness" more clearly, especially as transparency data becomes the backbone for public tools, payer negotiations, and compliance audits. Clear, standardized definitions help ensure consistent reporting across organizations, reducing disputes and enabling data to be trusted and actionable.
Tech vendors want a unified standard for both hospital and insurer files, while some provider groups argue the existing “good faith” standard is sufficient. One thing is consistent in their agreement: aligning data elements across hospitals, plans, and tools is foundational for true comparability.
2. Contract Complexity Challenges Data Accuracy
Many respondents, especially providers, flagged the difficulty of expressing a "standard charge" for services that are heavily dependent on variables like patient acuity, bundling, or discount structures. Actual payments often can't be known until after the fact. Despite these challenges, establishing a standard charge remains important for creating a consistent reference point that supports transparency, facilitates market comparisons, and informs policy and contracting decisions.
3. Emphasis on Patient-Friendly Tools over Raw Data Files
Hospitals and vendors alike noted that MRFs are not patient-facing tools and should not be treated as such. Instead, they advocated for a dual focus:
- Publish standardized files for compliance, analytics, and benchmarking
- Provide intuitive, shoppable tools that help patients estimate out-of-pocket costs
Patients shouldn't need to interpret all these spreadsheets. The burden of price bundling, packaging, and presentation should rest with providers and insurers.
4. Improving Data Completeness
Stakeholders pushed back on placeholder values and incomplete files, pushing CMS to require hospitals to publish real, knowable values for all services and charge types.
Many called on CMS to cross-verify provider files using insurer-posted data or existing claims databases that creates a feedback loop that prevents omissions.
5. Debate Over Enforcement Approach
Provider groups favor a collaborative enforcement model, pointing out that most compliance issues are minor and fixable. However, transparency advocates and some vendors pushed for more aggressive measures:
- Executive attestation of accuracy
- Treating false or missing data as a material misstatement
- Increased penalties for repeated noncompliance
6. Aligning and Streamlining Regulations
Many respondents called on CMS to reconcile the multiple and sometimes conflicting transparency requirements at the federal and state levels. Hospitals are juggling the Hospital Price Transparency rule, Transparency in Coverage rules for insurers, state-specific mandates, and elements of the No Surprises Act. This patchwork of requirements increases administrative burden and creates inconsistencies in how data is reported. Stakeholders urged CMS to harmonize formats, timelines, and data definitions to make compliance more manageable and to improve the comparability of data across markets.
7. The Growing Role of Third-Party Tools and Data Users
There was broad recognition that public price data is most valuable when it's put to work and not just posted online. Third-party entities, such as healthcare technology vendors, researchers, employer coalitions, and analytics firms, are already utilizing these files to benchmark prices, inform negotiations, and analyze market dynamics. These groups can amplify the benefits of transparency, but only if the data is clean, complete, and standardized. This emphasises the importance of improving accuracy and consistency in MRFs.
8. Support for Validation Tools and Guidance
Hospitals and tech vendors alike voiced support for resources that can catch errors and flag inconsistencies before files are even posted. Many pointed to CMS’s online MRF Validator as a helpful step in the right direction, while recommending enhancements like expanded automated checks, error explanations, and audit feedback loops. There is a shared goal to provide hospitals with the tools to self-correct and improve file quality proactively, thereby reducing the need for punitive enforcement after the fact.
9. Concerns About Burden and Requests for Stability
Compliance with evolving transparency regulations has required significant time, staffing, and financial investment from hospitals. When the initial rules went into effect, providers had to repeatedly adjust file formats and processes to keep up with new clarifications and requirements. Many stakeholders cautioned against introducing frequent changes going forward. Many argue that stability in the rules would allow hospitals to refine their processes and improve quality without constantly retooling their systems.
10. Focus on Payer Data and Cross-Market Transparency
Several respondents highlighted that hospital transparency data alone provides only part of the picture. Insurer-posted Transparency in Coverage (TiC) data offers the other half, capturing the payer’s perspective on negotiated rates. Stakeholders called for stronger alignment between hospital and insurer datasets, so that the two could be cross-verified and analyzed together. This would then create a more comprehensive and accurate view of market pricing benefiting regulators, researchers, and provider organizations seeking to understand their competitive position.
The takeaway? Expect sharper enforcement, especially if future legislation (like the Patients Deserve Price Tags Act) moves forward.
Sources:
.png)
White Paper
From Transparency to Prediction: Quantifying the Drivers of Physician Reimbursement Variation
This analysis uses Transparency in Coverage data to model how payers behave, not just what they pay. By linking reimbursement rates to physician characteristics, we uncover the patterns behind payment variation and transform transparency data into predictive intelligence. The result: a predictive view of rate dynamics that helps stakeholders anticipate trends and negotiate with data-driven confidence.

White Paper
Q3 2025 State of Commercial Reimbursement: Trek Health’s Quarterly Market Intelligence
Trek Health’s Quarterly Reimbursement Brief highlights emerging variability in commercial payment rates across U.S. payers, specialties, and geographic markets. With some segments experiencing double-digit growth and others notable declines, contracting performance is increasingly shaped by real-time payer behavior rather than historical norms. Through validated reimbursement trend analytics, contract intelligence, and policy monitoring, Trek equips provider organizations to anticipate market shifts, protect revenue, and negotiate with measurable leverage.

White Paper
Q4 2025 State of Commercial Reimbursement: Trek Health’s Quarterly Market Intelligence
Trek Health’s Q4 2025 Quarterly Market Intelligence report analyzes quarter-over-quarter commercial reimbursement movement across national payers, physician specialties, and U.S. states. While overall reimbursement improved following earlier declines, rate changes remained uneven—highlighting payer selectivity, persistent specialty outliers, and shifting geographic leverage. This report moves beyond static benchmarks by tracking real-time reimbursement changes, giving provider organizations actionable insight to identify negotiation risk early, protect rate parity, and respond proactively to evolving payer behavior.

White Paper
Reimbursement and Reality: The Economics of Breast Cancer Treatment
While breast cancer awareness efforts often focus on screening and treatment, one critical factor remains overlooked: how care is reimbursed. Payment structures shape far more than provider margins; they influence access, equity, and patient outcomes.
In this analysis of payer rates, Trek Health uses its Transparency Platform to analyze how reimbursement for breast cancer care varies across geography, commercial payer behavior, and public policy. The findings reveal a system that rewards disease burden rather than prevention which creates inequities that ripple through the entire care process.
Inside you’ll learn:
- How reimbursement rates differ dramatically by state and payer
- Why higher disease burden correlates with higher payment, but prevention does not
- What these trends mean for provider strategy, patient access, and equity
Download the full analysis to see how transparency data can help reshape breast cancer care—turning financial insight into fairer outcomes.

White Paper
The Payer Paradox: When Higher Rates Don’t Mean Higher Reimbursement
This analysis uncovers a critical paradox in commercial healthcare financing: the payers offering the highest contracted rates often deliver the lowest realized reimbursement once denials and administrative friction are accounted for. By introducing the Payer Generosity Index (PGI) and adjusted PGI (aPGI), Trek Health reveals how payer performance varies not only across insurers, but across specialties and service lines. These findings equip healthcare organizations with a clearer, data-driven framework for contracting, revenue optimization, and strategic planning in an increasingly complex reimbursement landscape.

White Paper
The Private Practice Playbook: Rate Negotiation Index Rankings for Specialty-Specific M&A Strategy
Physician economics are shifting as private equity and independent platforms redefine the workforce landscape. Trek Health’s Rate Negotiation Index Report quantifies the return on physician labor across states and specialties in a new lens: combining commercial reimbursement, physician salary, malpractice risk, and provider density into a single metric. This data driven foundation for smarter M&A strategy identifies the most economically sustainable opportunities across the U.S. for physician recruitment and network expansion.

Published on
August 12, 2025
Written by
The Top 10 CMS RFI Response Themes and What They Mean for Price Transparency
As CMS moves to refine and enforce hospital price transparency rules, the agency's Request for Information (RFI) drew an important response from stakeholders across the healthcare ecosystem. Hospitals, tech vendors, employers, patient advocates, and consultants all weighed in, and while not everyone agrees on the how, the what is clear: there's a new wave of transparency that prioritizes consistency, usability, and accountability.
Below, we break down the top 10 themes from the CMS RFI responses and what they signal for health systems trying to stay compliant, strategic, and ahead of enforcement.
1. Clarity in Definitions and Standardization
Across the board, stakeholders urged CMS to define key terms like "accuracy" and "completeness" more clearly, especially as transparency data becomes the backbone for public tools, payer negotiations, and compliance audits. Clear, standardized definitions help ensure consistent reporting across organizations, reducing disputes and enabling data to be trusted and actionable.
Tech vendors want a unified standard for both hospital and insurer files, while some provider groups argue the existing “good faith” standard is sufficient. One thing is consistent in their agreement: aligning data elements across hospitals, plans, and tools is foundational for true comparability.
2. Contract Complexity Challenges Data Accuracy
Many respondents, especially providers, flagged the difficulty of expressing a "standard charge" for services that are heavily dependent on variables like patient acuity, bundling, or discount structures. Actual payments often can't be known until after the fact. Despite these challenges, establishing a standard charge remains important for creating a consistent reference point that supports transparency, facilitates market comparisons, and informs policy and contracting decisions.
3. Emphasis on Patient-Friendly Tools over Raw Data Files
Hospitals and vendors alike noted that MRFs are not patient-facing tools and should not be treated as such. Instead, they advocated for a dual focus:
- Publish standardized files for compliance, analytics, and benchmarking
- Provide intuitive, shoppable tools that help patients estimate out-of-pocket costs
Patients shouldn't need to interpret all these spreadsheets. The burden of price bundling, packaging, and presentation should rest with providers and insurers.
4. Improving Data Completeness
Stakeholders pushed back on placeholder values and incomplete files, pushing CMS to require hospitals to publish real, knowable values for all services and charge types.
Many called on CMS to cross-verify provider files using insurer-posted data or existing claims databases that creates a feedback loop that prevents omissions.
5. Debate Over Enforcement Approach
Provider groups favor a collaborative enforcement model, pointing out that most compliance issues are minor and fixable. However, transparency advocates and some vendors pushed for more aggressive measures:
- Executive attestation of accuracy
- Treating false or missing data as a material misstatement
- Increased penalties for repeated noncompliance
6. Aligning and Streamlining Regulations
Many respondents called on CMS to reconcile the multiple and sometimes conflicting transparency requirements at the federal and state levels. Hospitals are juggling the Hospital Price Transparency rule, Transparency in Coverage rules for insurers, state-specific mandates, and elements of the No Surprises Act. This patchwork of requirements increases administrative burden and creates inconsistencies in how data is reported. Stakeholders urged CMS to harmonize formats, timelines, and data definitions to make compliance more manageable and to improve the comparability of data across markets.
7. The Growing Role of Third-Party Tools and Data Users
There was broad recognition that public price data is most valuable when it's put to work and not just posted online. Third-party entities, such as healthcare technology vendors, researchers, employer coalitions, and analytics firms, are already utilizing these files to benchmark prices, inform negotiations, and analyze market dynamics. These groups can amplify the benefits of transparency, but only if the data is clean, complete, and standardized. This emphasises the importance of improving accuracy and consistency in MRFs.
8. Support for Validation Tools and Guidance
Hospitals and tech vendors alike voiced support for resources that can catch errors and flag inconsistencies before files are even posted. Many pointed to CMS’s online MRF Validator as a helpful step in the right direction, while recommending enhancements like expanded automated checks, error explanations, and audit feedback loops. There is a shared goal to provide hospitals with the tools to self-correct and improve file quality proactively, thereby reducing the need for punitive enforcement after the fact.
9. Concerns About Burden and Requests for Stability
Compliance with evolving transparency regulations has required significant time, staffing, and financial investment from hospitals. When the initial rules went into effect, providers had to repeatedly adjust file formats and processes to keep up with new clarifications and requirements. Many stakeholders cautioned against introducing frequent changes going forward. Many argue that stability in the rules would allow hospitals to refine their processes and improve quality without constantly retooling their systems.
10. Focus on Payer Data and Cross-Market Transparency
Several respondents highlighted that hospital transparency data alone provides only part of the picture. Insurer-posted Transparency in Coverage (TiC) data offers the other half, capturing the payer’s perspective on negotiated rates. Stakeholders called for stronger alignment between hospital and insurer datasets, so that the two could be cross-verified and analyzed together. This would then create a more comprehensive and accurate view of market pricing benefiting regulators, researchers, and provider organizations seeking to understand their competitive position.
The takeaway? Expect sharper enforcement, especially if future legislation (like the Patients Deserve Price Tags Act) moves forward.
Sources:

